Introduction & Etiology
Temporomandibular Joint Disorder (TMD) describes a complex group of muscular and articular disorders affecting the TMJ, leading to pain, dysfunction, and eventually degeneration.
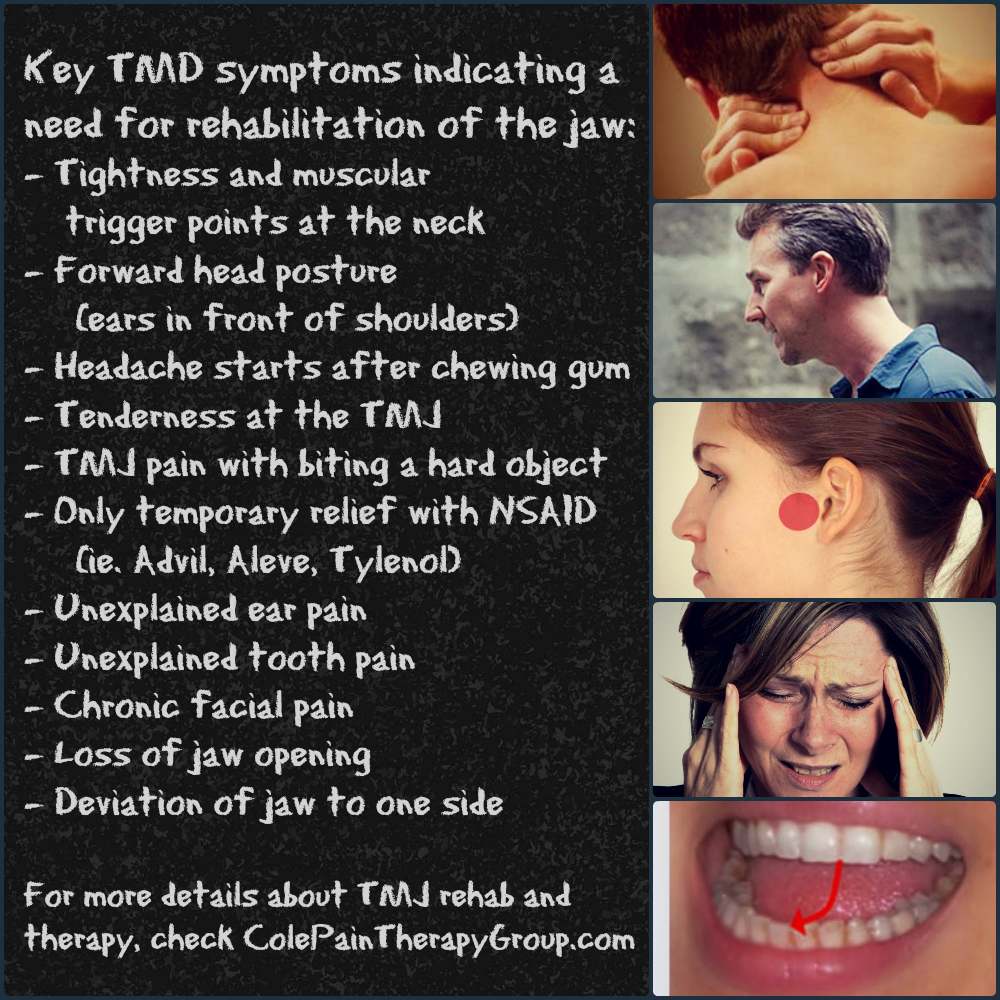
Most causes of TMD can be divided into either myogenous (muscular) or arthrogenous (articular). TMD of myogenous origin is more common (1) and may arise from muscular hypertonicity, trigger points, fascial restrictions, and/or functional muscle imbalance of the muscles of mastication. One of the most commonly involved muscles is the masseter. Other recognized triggers for myogenous TMD include bruxism, clenching, cervicocranial dysfunction (2), postural syndromes, especially a forward head posture (3,4,100), and trauma (5). TMD symptoms may occur in up to one-third of those patients involved in a whiplash injury. (6).
Disk displacement and osteoarthritis are common causes for TMD of arthrogenous origin. Other causes of TMD of articular origin include loose bodies, inflammatory arthropathy, trauma, mandibular fracture, dislocation, malocclusion, infection, and neoplasm. In TMD of articular origin, muscular dysfunction is secondary.
Studies vary on the relationship of premolar extraction to the development of TMD (7). Still, a systematic review suggests that the third molar location, degree of impaction, and subsequent extraction are associated with the development of TMD. (57). Nail biting, grinding of teeth, biting of lips, mouth breathing, and playing a musical instrument are significantly associated with TMD symptoms. (39,86) Being overweight or having poor physical fitness are known risk factors for TMD symptoms. (82) Sleeping less than 5 hours or greater than 9 hours each night is associated with an increased rate of TMD. (80,89) The incidence of TMD is higher in patients with untreated sleep apnea. (77) Age and Previous Orthodontics treatment have not been linked to TMD. (106)
Psychosocial disturbances, including stress and depression, are another widely recognized co-morbidity for TMD. (46,81,84,93,110,113) Stress alone has been identified as the most significant factor in developing TMD. (99) TMD patients with PTSD report a nearly four-fold increase in pain as compared to subjects without PTSD. (42) Patients with polycystic ovary syndrome are nearly seven times more likely to suffer from TMD. (69) Ankylosing spondylitis patients have a nearly three-fold increased risk. (85,90,120) TMD patients have an elevated incidence of suffering from migraine headaches. (59)
Estimates for the incidence of TMD vary between 4-31% (8,9,73). Up to 3% of Americans seek treatment for TMD each year (21). At presentation, most patients are 20-50 years old, and prevalence is 2-3 times higher in females. Patients with rheumatoid arthritis have a higher incidence of TMD. (60,73)
Clinical Presentation
Typical symptoms include clicking or crepitus, restricted opening, transient locking, and pain. Symptoms may be exacerbated by mastication. TMD pain is generally described as an “ache” located immediately anterior to the ear canal but may refer to other areas of the face, head, neck and shoulders. (6) Spinal pain and tenderness are common concurrent findings in TMD patients. (43,45) Up to half of TMD patients concurrently suffer from neck pain and headaches, suggesting a common link arising from the upper cervical spine. (10,37,74,88,101,102) Decreased glenoid fossa depth may be associated with an increased incidence of tinnitus in TMD patients due to their close anatomical relationship. (104) In addition to tinnitus, other otologic signs/symptoms include ear fullness, otalgia, vertigo, or hearing loss. These symptoms occur with TMD concurrently 85–95% of the time. (115) Patients with chronic TMD frequent stomach pain has been observed. (88) Patients with painful TMD frequently report sleep disturbances. (51) The Fonseca Anamnestic Index provides a list of screening questions to identify and quantify the severity of TMD. (63-67)
Clinicians should be particularly vigilant for cardiac origins of jaw pain, particularly in higher-risk populations. A TMD consensus panel identified the following functional assessments as the most useful for identifying TMD: Jaw Functional Limitation (JFL-8), Mandibular Function Impairment Questionnaire (MFIQ), Tampa Scale for Kinesiophobia for Temporomandibular disorders (TSK/TMD), and the Neck Disability Index (NDI). (48)
Clinical evaluation for TMD should include visual and palpatory assessment of the opening pattern (mouth opening test), while observing lateral deviation and “jerky” movements. (48) Vertical interincisal opening of less than 40mm is considered restricted. (11) Congenitally missing tooth is the most common dental abnormality and is a risk factor for TMD (117) Clinicians should assess for audible or palpable joint clicking or crepitus of the TMJ upon opening and closing. (48) TMD patients tend to exhibit a hypolordotic or kyphotic neck posture. (50) Cervical spine muscle weakness and hypomobility are common in TMD patients. (70,75) TMD patients often exhibit cervical spine motion limitations, particularly in the upper segments. (54,55)
Palpation may reveal tenderness in the: suboccipitals, temporalis, masseter, anterior and posterior digastrics, pterygoids, SCM and trapezius. Intersegmental mobility of the cervicocranial junction, cervical spine, and upper thoracic spine should be assessed. Hyoid mobility is assessed by moving the hyoid side to side in a supine patient. Limited or asymmetric hyoid mobility suggests digastric tension. Orthopedic evaluation should also include the centric relation provocation test, which tests the disc-condyle complex in the most stable position. Since the disc is not innervated, compression of the mandible into the temporal fossa should not elicit symptoms in healthy joints. Reproduction of pain means the condyle is contacting the fossa, suggesting a structural pathology (i.e. disc dislocation, osteoarthritis, or capsulitis).
Diagnostics & Differential
In many cases, TMD cannot be assessed by clinical evaluation alone. Panoramic x-rays are of limited help in identifying articular causes of TMD. CT is the imaging of choice (over 4 times better than plain films) for identifying TMJ osteoarthritis. Advanced imaging signs of TMD include disc displacement/ deformation, joint effusion, osteoarthritis, and increased thickness of roof of glenoid fossa. (38,58,61) Current studies with CT also indicated a likely relationship between mandibular asymmetries and TMD. (91) The reliability of MRI is excellent for detecting disc displacements and effusion. (12) Diagnostic ultrasound is a non-invasive modality that is less expensive and does not demand special facilities while producing dynamic images with good identification of disc displacement. (33,105) Patients with TMD do not demonstrate significant EMG variations as compared to healthy controls. (47)
The differential diagnosis of TMD would include disc displacement, degeneration, fracture, infection (i.e., parotid gland, tooth), dental pathology, neoplasm, trigeminal neuralgia, and cardiogenic referral.
Management
Non-surgical intervention for TMD has been shown to be as effective as any surgical intervention. (13,108,122) Management should be conservative and simple, focusing on three main points: manual therapies, exercise, and avoidance of aggravating activities. (52) Muscle energy technique and occlusal splint therapy as a combined therapy were shown to significantly reduce pain and improve mouth opening. (92)
Manual therapy has varied support as an effective treatment for TMD. (30,49,52,68,83,121,123) Upper cervical manipulation appeared to have the most impact in decreasing symptoms of TMD with manual therapy. (107,119) Manual therapies may be necessary to address lesions in the masticatory system, neck and upper torso. Intraoral myofascial therapy has been shown to reduce pain and improve jaw opening. (29) Post-isometric relaxation (PIR), STM, or myofascial release should be directed at the: lateral pterygoid, temporalis, and masseter. (14,15) Other muscles that may need consideration include the: suboccipitals, anterior and posterior digastrics, medial pterygoid, SCM, and trapezius. (72)
TMJ non-thrust mobilization is often indicated (10) and may be performed by grasping the jaw with the clinician’s thumbs on the molars, applying distraction, and moving the jaw in a figure-eight clockwise or counterclockwise fashion for 20 repetitions. HVLA manipulation of the jaw is controversial and shows only limited short-term benefit. (32) Manipulation of the cervicocranial, cervical, and thoracic spine may be helpful. (16,44) Upper cervical manipulation has demonstrated benefit in chronic TMD cases. (36) Chiropractic cervical spine manipulation has been shown to increase maximal bite force. (31) Before conducting cervical manipulation, providers should screen for potential contraindications.
Exercises to improve posture and TMJ function have been shown to be beneficial (10,17,18,52,83,97,112,114,118,121). Stretching exercises should address tightness in the masseter, SCM, levator and suboccipitals. The patient should also perform chin retractions, deep neck flexion and chin depression. Additional postural corrections may be necessary, particularly for deep neck flexor weakness. (75,124). The Rocabado 6×6 exercise protocol is a popular program to restore function between the jaw, neck, and shoulders. (22) In contrast to popular opinion, some experts suggest that management of malocclusion is not essential in the treatment of TMD. (19)
Initially, passive modalities including, heat, ice, ultrasound, or iontophoresis may be helpful. (20,28,35,40) One systematic review concluded that laser therapy is helpful for TMD. (61) Extracorporeal Shockwave Therapy (ESWT) has demonstrated benefit for TMD patients. (53) Acupuncture has been shown to reduce pain in TMD patients. (55,76) Laser acupuncture and low-level diode laser therapy were shown to have similar efficacy in the treatment of the myofascial pain of TMD. (98,103) Localized vibration therapy may provide pain relief. (71) Microcurrent Electrical Nerve Stimulation [MENS] therapy is an effective non-invasive treatment that can be used to reduce pain in patients with myofascial pain of the masticatory muscle. (94,96) TENS and high voltage currents are also valid options for the control of pain intensity in patients suffering from temporomandibular disorder. although the quality of evidence supporting this study was considered low. (116)
Patients should avoid aggravating activities like chewing gum or eating “rubbery” foods. Patients should limit unnecessary talking. (18,19) Home education should include instruction on how to maintain a relaxed jaw position. (79) Glucosamine and chondroitin sulfate have shown success in managing TMD. (34) Supplementation with bromelain or MSM may also be beneficial. A gluten-free diet was shown to be effective in reducing chronic myofascial pain in masticatory muscles. (87) A custom-fitted mouthguard (occlusal orthotic) may help minimize grinding or clenching and promote relaxation of masticatory muscles. (20) Patients with nighttime symptoms should avoid stressful activity before bedtime and be aware of their sleep position. NSAIDs may provide benefit. Patients with TMD typically have higher anxiety levels and lower quality of life scores. (41) Long-term strategies should address any biopsychosocial factors. There is an increased probability of TMD among patients with a history of certain mental and behavioral disorders, and a stronger association with TMD requiring surgery, specifically repeated surgery. (109) The addition of modern Pain Science Education (PSE) intervention improved disability for people with chronic TMD receiving manual therapy and exercise. (111) In some cases, stress management techniques, like biofeedback, can assist patients in learning how to relax the jaw muscles. Stem cell therapy may provide benefits for damaged TMJ components. (78)
References
- Fricton JR. Temporomandibular muscle and joint disorders. Pain. 2004 Jun;109:530.
- Catanzariti JF, Debuse T, Duquesnoy B. Chronic neck pain and masticatory dysfunction. Joint Bone Spine. 2005 Dec 1;72(6):515-9. Link
- Palazzi C, Miralles R, Soto MA, Santander H, Zuñiga C, Moya H. Body position effects on EMG activity of sternocleidomastoid and masseter muscles in patients with myogenic cranio-cervical-mandibular dysfunction. CRANIO®. 1996 Jul 1;14(3):200-9. Link
- Gonzalez HE, Manns A. Forward head posture: its structural and functional influence on the stomatognathic system, a conceptual study. CRANIO®. 1996 Jan 1;14(1):71-80. Link
- Yun PY, Kim YK. The role of facial trauma as a possible etiologic factor in temporomandibular joint disorder. Journal of oral and maxillofacial surgery. 2005 Nov 1;63(11):1576-83. Link
- Salé H, Isberg A. Delayed temporomandibular joint pain and dysfunction induced by whiplash trauma: a controlled prospective study. The Journal of the American Dental Association. 2007 Aug 1;138(8):1084-91. Link
- Egermark I, Thilander B. Craniomandibular disorders with special reference to orthodontic treatment: an evaluation from childhood to adulthood. American Journal of Orthodontics and Dentofacial Orthopedics. 1992 Jan 1;101(1):28-34. Link
- Gremillion HA, Mahan PE: The prevalence and etiology of temporomandibular disorders and orofacial pain. Tex Dent J 2000; 117:30-39.
- Von Korff M, Dworkin SF, LeResche L, et al: An epidemiologic comparison of pain complaints. Pain 1988;32(2):173-183.
- Furto ES, Cleland JA, Whitman JM, Olson KA. Manual physical therapy interventions and exercise for patients with temporomandibular disorders. CRANIO®. 2006 Oct 1;24(4):283-91. Link
- Feteih RM. Signs and symptoms of temporomandibular disorders and oral parafunctions in urban Saudi Arabian adolescents: a research report. Head & face medicine. 2006 Dec;2(1):25. Link
- Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Truelove EL, John MT, Schiffman EL. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2009 Jun 1;107(6):844-60. Link
- Fricton JR, Look JO, Schiffman E, Swift J. Long-term study of temporomandibular joint surgery with alloplastic implants compared with nonimplant surgery and nonsurgical rehabilitation for painful temporomandibular joint disc displacement. Journal of oral and maxillofacial surgery. 2002 Dec 1;60(12):1400-11. Link
- Blanco CR, de las Peñas CF, Xumet JE, Algaba CP, Rabadán MF, de la Quintana MC. Changes in active mouth opening following a single treatment of latent myofascial trigger points in the masseter muscle involving post-isometric relaxation or strain/counterstrain. Journal of bodywork and movement therapies. 2006 Jul 1;10(3):197-205. Link
- Kalamir A, Bonello R, Graham P, Vitiello AL, Pollard H. Intraoral myofascial therapy for chronic myogenous temporomandibular disorder: a randomized controlled trial. Journal of manipulative and physiological therapeutics. 2012 Jan 1;35(1):26-37. Link
- Pilar Mansilla-Ferragut, DO, César Fernández-de-las Peñas, DO, PhD, Francisco Alburquerque-Sendi`n, DO, PhD, Joshua A. Cleland, PhD, and Juan José Boscá-Gandi. DO J Manipulative Physiol Ther 2009;32:101-106
- Nicolakis P, Burak EC, Kollmitzer J, Kopf A, Piehslinger E, Wiesinger GF, Fialka-Moser V. An investigation of the effectiveness of exercise and manual therapy in treating symptoms of TMJ osteoarthritis. CRANIO®. 2001 Jan 1;19(1):26-32. Link
- Gavish A, Winocur E, Astandzelov-Nachmias T, Gazit E. Effect of controlled masticatory exercise on pain and muscle performance in myofascial pain patients: a pilot study. CRANIO®. 2006 Jul 1;24(3):184-90. Link
- Skaggs C. TMJ dysfunction. Journal of Bodywork and Movement Therapy. 1997;1(4):198-214.
- Wright EF, North SL. Management and treatment of temporomandibular disorders: a clinical perspective. Journal of Manual & Manipulative Therapy. 2009 Dec 1;17(4):247-54. Link
- Drangsholt M, LeResche L. In: Temporomandibular disorder pain. In: Epidemiology of pain. Crombie IK, Croft PR, Linton SJ, LeResche L, Von Korff M, editors. IASP Press; Seattle: 1999. pp. 203–233
- Rocabado M. Diagnosis and treatment of abnormal craniocervical and craniomandibular mechanics. Abnormal Jaw Mechanics: Diagnosis and Treatment. Chicago: Quintessenz. 1984:141-9.
- Pereira TS, Flecha OD, Guimaraes RC, Oliveira DD, Botelho AM, Glória JC, Tavano KT. Efficacy of red and infrared lasers in treatment of temporomandibular disorders—a double-blind, randomized, parallel clinical trial. CRANIO®. 2014 Jan 1;32(1):51-6. Link
- Randhawa K, et al. The effectiveness of non-invasive interventions for temporomandibular disorders: A systematic review by the ontario protocol for traffic injury management (optima) collaboration. Clin J Pain. 2015 Apr 28.
- Martins WR, Blasczyk JC, de Oliveira MA, Gonçalves KF, Bonini-Rocha AC, Dugailly PM, de Oliveira RJ. Efficacy of musculoskeletal manual approach in the treatment of temporomandibular joint disorder: A systematic review with meta-analysis. Manual therapy. 2016 Feb 1;21:10-7. Link
- Haavik H, Özyurt M, Niazi I, Holt K, Nedergaard R, Yilmaz G, Türker K. Chiropractic manipulation increases maximal bite force in healthy individuals. Brain sciences. 2018 May;8(5):76. Link
- Nagata K, Hori S, Mizuhashi R, Yokoe T, Atsumi Y, Nagai W, Goto M. Efficacy of mandibular manipulation technique for temporomandibular disorders patients with mouth opening limitation: a randomized controlled trial for comparison with improved multimodal therapy. Journal of prosthodontic research. 2019;63(2):202-9. Link
- Pekince KA, Ça?layan F, Pekince A. The efficacy and limitations of USI for diagnosing TMJ internal derangements. Oral Radiology. 2020 Jan 1;36(1):32-9. Link
- Ganti S, Shriram P, Ansari AS, Kapadia JM, Azad A, Dubey A. Evaluation of Effect of Glucosamine-Chondroitin Sulfate, Tramadol, and Sodium Hyaluronic Acid on Expression of Cytokine Levels in Internal Derangement of Temporomandibular Joint. The journal of contemporary dental practice. 2018 Dec 1;19(12):1501-5. Link
- Madani A, Ahrari F, Fallahrastegar A, Daghestani N. A randomized clinical trial comparing the efficacy of low-level laser therapy (LLLT) and laser acupuncture therapy (LAT) in patients with temporomandibular disorders. Lasers in Medical Science. 2019 Aug 8:1-2.
- Corum M, Basoglu C, Topaloglu M, Diracoglu D, Aksoy C. Spinal high-velocity low-amplitude manipulation with exercise in women with chronic temporomandibular disorders. Manuelle Medizin. 2018 Jun 1;56(3):230-8. Link
- Plesh O, Adams SH, Gansky SA (2011) Temporomandibular Joint and Muscle Disorder (TMJMD)-type pain and Co-morbid pains in a National US Sample. J Orofac Pain 25:190 Link
- Khojastepour L, Haghnegahdar A, Eisazadeh M, Bahreini M. Comparison between Glenoid Fossa Roof Thickness in TMD and non-TMD Patients, a CBCT Study. J Dent (Shiraz). 2019;20(3):165–170. Link
- Chaulagain R, Maharjan A. Prevalence of Temporomandibular Joint Disorders and its Association with Para Functional Habits in the Patients Attending Tertiary Care Hospital. Journal of Nepal Health Research Council. 2019 Nov 13;17(3):376-81. Link
- Khairnar S, Bhate K, SN SK, Kshirsagar K, Jagtap B, Kakodkar P. Comparative evaluation of low-level laser therapy and ultrasound heat therapy in reducing temporomandibular joint disorder pain. Journal of dental anesthesia and pain medicine. 2019 Oct 1;19(5):289-94. Link
- de Resende CM, da Silva Rocha LG, de Paiva RP, da Silva Cavalcanti C, de Almeida EO, Roncalli AG, Barbosa GA. Relationship between anxiety, quality of life, and sociodemographic characteristics and temporomandibular disorder. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 2019 Nov 26. Link
- Kindler S, Schwahn C, Bernhardt O, Söhnel A, Mksoud M, Biffar R, Meyer G, Völzke H, Metelmann HR, Grabe HJ. Association Between Symptoms of Posttraumatic Stress Disorder and Signs of Temporomandibular Disorders in the General Population. Journal of Oral & Facial Pain & Headache. 2019 Jan 1;33(1). Link
- Kim D, Ko SG, Lee EK, Jung B. The relationship between spinal pain and temporomandibular joint disorders in Korea: a nationwide propensity score-matched study. BMC Musculoskeletal Disorders. 2019 Dec;20(1):1-3. Link
- Reynolds B, Puentedura EJ, Kolber MJ, Cleland JA. Effectiveness of cervical spine high velocity low amplitude thrust added to behavioral education, soft tissue mobilization, and exercise in individuals with temporomandibular disorder (TMD) with myalgia: A randomized clinical trial. Journal of Orthopaedic & Sports Physical Therapy. 2020 Jan 6(0):1-40. Link
- Almoznino G, Zini A, Zakuto A, Zlutzky H, Bekker S, Shay B, Haviv Y, Sharav Y, Benoliel R. Cervical Muscle Tenderness in Temporomandibular Disorders and Its Associations with Diagnosis, Disease-Related Outcomes, and Comorbid Pain Conditions. Journal of oral & facial pain and headache. 2019 Aug. Link
- Alahmary AW. Association of Temporomandibular Disorder Symptoms with Anxiety and Depression in Saudi Dental Students. Open Access Macedonian Journal of Medical Sciences. 2019 Dec 15;7(23):4116.
- Massaroto Barros B, Biasotto-Gonzalez DA, Bussadori SK, Gomes CA, Politti F. Is there a difference in the electromyographic activity of the masticatory muscles between individuals with temporomandibular disorder and healthy controls? A systematic review with meta-analysis. Journal of Oral Rehabilitation. Link
- von Piekartz H, Schwiddessen J, Reineke L, Armijo?Olivio S, Bevilaqua?Grossi D, Biasotto Gonzalez DA, Carvalho G, Chaput E, Cox E, Fernández?de?las?Peñas C, Gadotti IC. International consensus on the most useful assessments used by physical therapists to evaluate patients with temporomandibular disorders: A Delphi study. Journal of Oral Rehabilitation. 2020 Jun;47(6):685-702. Link
- de Melo LA, Bezerra de Medeiros AK, Campos MF, de Resende BM, Barbosa GA, de Almeida EO. Manual Therapy in the Treatment of Myofascial Pain Related to Temporomandibular Disorders: A Systematic Review. Journal of Oral & Facial Pain and Headache. 2020 Mar 1;34(2):141-8. Link
- Coskun Benlidayi I, Guzel R, Tatli U, Salimov F, Keceli O. The relationship between neck pain and cervical alignment in patients with temporomandibular disorders. CRANIO®. 2020 May 3;38(3):174-9. Link
- Dreweck FD, Soares S, Duarte J, Conti PC, De Luca Canto G, Porporatti AL. Association between painful temporomandibular disorders and sleep quality: A systematic review. Journal of Oral Rehabilitation. 2020 May 12. Link
- La Touche R, Boo-Mallo T, Zarzosa-Rodríguez J, Paris-Alemany A, Cuenca-Martínez F, Suso-Martí L. Manual therapy and exercise in temporomandibular joint disc displacement without reduction. A systematic review. CRANIO®. 2020 Jun 28:1-1. Link
- Li W, Wu J. Treatment of Temporomandibular Joint Disorders by Ultrashort Wave and Extracorporeal Shock Wave: A Comparative Study. Medical Science Monitor. 2020 Jun 21;26. Link
- Micarelli A, Viziano A, Granito I, Micarelli RX, Augimeri I, Alessandrini M. Temporomandibular disorders and cervicogenic dizziness: Relations between cervical range of motion and clinical parameters. CRANIO®. 2020 Jun 17:1-0. Link
- Sen S, Orhan G, Sertel S, Schmitter M, Schindler HJ, Lux CJ, Giannakopoulos NN. Comparison of acupuncture on specific and non?specific points for the treatment of painful temporomandibular disorders: A randomised controlled trial. Journal of Oral Rehabilitation. 2020 Feb 20. Link
- Greenbaum T, Dvir Z, Emodi-Perelmam A, Reiter S, Rubin P, Winocur E. Relationship between specific temporomandibular disorders and impaired upper neck performance. European Journal of Oral Sciences. 2020. Link
- Damasceno YS, Espinosa DG, Normando D. Is the extraction of third molars a risk factor for the temporomandibular disorders? A systematic review. Clinical Oral Investigations. 2020 Aug 10:1-0. Link
- Jerele C, Avsenik J, Popovi KŠ. MRI characteristics of the asymptomatic temporomandibular joint in patients with unilateral temporomandibular joint disorder. Oral Radiology. 2020 Sep 18:1-7. Link
- Byun SH, Min C, Yoo DM, Yang BE, Choi HG. Increased Risk of Migraine in Patients with Temporomandibular Disorder: A Longitudinal Follow-Up Study Using a National Health Screening Cohort. Diagnostics. 2020 Sep;10(9):724. Link
- Byun SH, Min C, Choi HG, Hong SJ. Increased Risk of Temporomandibular Joint Disorder in Patients with Rheumatoid Arthritis: A Longitudinal Follow-Up Study. Journal of Clinical Medicine. 2020 Sep;9(9):3005. Link
- Alzahrani A, Yadav S, Gandhi V, Lurie AG, Tadinada A. Incidental findings of temporomandibular joint osteoarthritis and its variability based on age and sex. Imaging Science in Dentistry. 2020 Sep;50(3):245. Link
- Zwiri A, Alrawashdeh MA, Khan M, Ahmad WM, Kassim NK, Ahmed Asif J, Suan Phaik K, Husein A, Ab-Ghani Z. Effectiveness of the Laser Application in Temporomandibular Joint Disorder: A Systematic Review of 1172 Patients. Pain Research and Management. 2020 Sep 11;2020. Link
- Fonseca D.M. Disfunção temporomandibular (DTM): elaboração de um índice anamnésico. J Appl Oral Sci. 1992
- Fonseca DM, Bonfante G, Valle AL, Freitas SF. Diagnosis by anamnesis of craniomandibular dysfunction. RGO (Porto Alegre). 1994: 23-8. Link
- dos Santos Berni KC, Dibai-Filho AV, Rodrigues-Bigaton D. Accuracy of the Fonseca anamnestic index in the identification of myogenous temporomandibular disorder in female community cases. Journal of bodywork and movement therapies. 2015 Jul 1;19(3):404-9. Link
- Visscher CM, Naeije M, De Laat A, Michelotti A, Nilner M, Craane B, Ekberg E, Farella M, Lobbezoo F. Diagnostic accuracy of temporomandibular disorder pain tests: a multicenter study. Journal of orofacial pain. 2009 Apr 1;23(2). Link
- Stasiak G, Maracci LM, de Oliveira Chami V, Pereira DD, Tomazoni F, Bernardon Silva T, Ferrazzo V, Marquezan M. TMD diagnosis: Sensitivity and specificity of the Fonseca Anamnestic Index. CRANIO®. 2020 Oct 29:1-5. Link
- Herrera-Valencia A, Ruiz-Muñoz M, Martin-Martin J, Cuesta-Vargas A, González-Sánchez M. Efficacy of Manual Therapy in Temporomandibular Joint Disorders and Its Medium-and Long-Term Effects on Pain and Maximum Mouth Opening: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2020 Nov;9(11):3404. Link
- Yazici H, Taskin MI, Guney G, Hismiogullari AA, Arslan E, Tulaci KG. The novel relationship between Polycystic Ovary Syndrome and Temporomandibular Joint Disorders. Journal of Stomatology, Oral and Maxillofacial Surgery. 2020 Nov 5. Link
- de Oliveira-Souza AI, Ferro JK, Barros MM, de Oliveira DA. Cervical musculoskeletal disorders in patients with temporomandibular dysfunction: A systematic review and meta-analysis. Journal of Bodywork and Movement Therapies. 2020 May 11. Link
- Serritella E, Scialanca G, Di Giacomo P, Di Paolo C. Local Vibratory Stimulation for Temporomandibular Disorder Myofascial Pain Treatment: A Randomised, Double-Blind, Placebo-Controlled Preliminary Study. Pain Research and Management. 2020 Dec 5;2020. Link
- Ku J, Szarejko KD, Gobiewska M. Evaluation of Soft Tissue Mobilization in Patients with Temporomandibular Disorder-Myofascial Pain with Referral. International Journal of Environmental Research and Public Health. 2020 Jan;17(24):9576. Link
- Valesan LF, Da-Cas CD, Réus JC, Denardin AC, Garanhani RR, Bonotto D, Januzzi E, de Souza BD. Prevalence of temporomandibular joint disorders: a systematic review and meta-analysis. Clinical Oral Investigations.:1-3. Link
- Greenbaum T, Dvir Z, Emodi-Perlman A, Reiter S, Rubin P, Winocur E. The association between specific temporomandibular disorders and cervicogenic headache. Musculoskeletal Science and Practice.:102321. Link
- Greenbaum T, Dvir Z, Emodi?Perelmam A, Reiter S, Rubin P, Winocur E. Relationship between specific temporomandibular disorders and impaired upper neck performance. European journal of oral sciences. 2020 Aug;128(4):292-8. Link
- Katekawa L, Iwasaki AC, Shinkai RS, de Campos TT. Acupuncture applied at local or distal acupoints reduces pain related to temporomandibular disorders in female patients. The International Journal of Prosthodontics. 2021 Feb 19. Link
- Alessandri-Bonetti A, Scarano E, Fiorita A, Cordaro M, Gallenzi P. Prevalence of signs and symptoms of temporo-mandibular disorder in patients with sleep apnea. Sleep and Breathing. 2021 Mar 5:1-6. Link
- Pagotto LE, de Santana Santos T, Pastore GP. The efficacy of mesenchymal stem cells in regenerating structures associated with the temporomandibular joint: a systematic review. Archives of Oral Biology. 2021 Mar 6:105104. Link
- Xu L, Zhang L, Lu J, Fan S, Cai B, Dai K. Head and neck posture influences masticatory muscle electromyographic amplitude in healthy subjects and patients with temporomandibular disorder: a preliminary study. Annals of Palliative Medicine. 2021 Mar 3. Link
- Hyungkil Choi DD, Hye-Young Sim DD, Kyoung-In Yun DD. Association between sleeping time and temporomandibular disorders in a sample of the South Korean population. CRANIO®. 2019 Mar 21. Link
- Yap AU, Marpaung C, Rahmadini ED. Psychological well-being and distress: Their associations with Temporomandibular disorder symptoms and inter-relationships. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 2021 Feb 24. Link
- Miettinen O, Kämppi A, Tanner T, Anttonen V, Patinen P, Päkkilä J, Tjäderhane L, Sipilä K. Association of Temporomandibular Disorder Symptoms with Physical Fitness among Finnish Conscripts. International Journal of Environmental Research and Public Health. 2021 Jan;18(6):3032. Link
- Tanhan A, Ozer AY, Polat MG. Efficacy of different combinations of physiotherapy techniques compared to exercise and patient education in temporomandibular disorders: A randomized controlled study. CRANIO®. 2021 Apr 6:1-3. Link
- Lei J, Yap AU, Zhang M, Fu KY. Temporomandibular disorder subtypes, emotional distress, impaired sleep, and oral health-related quality of life in Asian patients. Community dentistry and oral epidemiology. 2021 Apr 7. Link
- Huang YF, Chang CT, Muo CH, Chiu KM, Tsai CH, Liu SP. Bidirectional relationship between temporomandibular disorder and ankylosing spondylitis: a population-based cohort study. Clinical Oral Investigations. 2021 Apr 14:1-8. Link
- Campos LG, Pedrosa BH, Cavalcanti RV, Stechman?Neto J, Gadotti IC, de Araujo CM, Taveira KV. Prevalence of temporomandibular disorders in musicians: A systematic review and meta?analysis. Journal of Oral Rehabilitation. 2021 Jan 20. Link
- Araújo Oliveira Buosi J, Abreu Nogueira SM, Pinheiro Sousa M, Costa Maia CS, Rocha Regis R, Matthes de Freitas Pontes K, Rigoldi Bonjardim L, Sales Pinto Fiamengui LM. Gluten-Free Diet Reduces Pain in Women with Myofascial Pain in Masticatory Muscles: A Preliminary Randomized Controlled Trial. Journal of Oral & Facial Pain & Headache. 2021 Jul 1;35(3). Link
- Velly AM, Botros J, Bolla MM, Khan K, Teixeira Junior OA, Guimarães AS, Gornitsky M. Painful and non?painful comorbidities associated with short?and long?term painful temporomandibular disorders: A cross?sectional study among adolescents from Brazil, Canada, and France. Journal of Oral Rehabilitation. Link
- Roithmann CC, Silva CA, Pattussi MP, Grossi ML. Subjective sleep quality and temporomandibular disorders: Systematic literature review and meta?analysis. Journal of Oral Rehabilitation. 2021 Dec;48(12):1380-94. Link
- Souza RC, de Sousa ET, Sousa D, Sales M, dos Santos Oliveira R, Mariano MH, Rushansky E, Gomes AC, Silva E. Prevalence of Temporomandibular Joint Disorders in Patients with Ankylosing Spondylitis: A Cross-Sectional Study. Clinical, Cosmetic and Investigational Dentistry. 2021;13:469. Link
- Alqhtani N, Alshammery D, AlOtaibi N, AlZamil F, Allaboon A, AlTuwaijri D, Baseer MA. Correlations between mandibular asymmetries and temporomandibular disorders: A systematic review. Journal of International Society of Preventive & Community Dentistry. 2021 Sep;11(5):481. Link
- Ram HK, Shah DN. Comparative evaluation of occlusal splint therapy and muscle energy technique in the management of temporomandibular disorders: A randomized controlled clinical trial. The Journal of Indian Prosthodontic Society. 2021 Oct 1;21(4):356. Link
- Kleykamp BA, Ferguson MC, McNicol E, Bixho I, Arnold LM, Edwards RR, Fillingim R, Grol-Prokopczyk H, Ohrbach R, Turk DC, Dworkin RH. The prevalence of comorbid chronic pain conditions among patients with temporomandibular disorders: A systematic review. The Journal of the American Dental Association. 2021 Dec 21. Link
- Bavarian R, Khawaja SN, Ajisafe AH, Sultan AS. The efficacy of microcurrent electrical nerve stimulation in treating masticatory myofascial pain: A systematic review and meta-analysis. CRANIO®. 2021 Dec 24:1-7. Link
- Mustafa MA, Al-Attas BA, Badr FF, Jadu FM, Wali SO, Bawazir YM. Prevalence and Severity of Temporomandibular Disorders in Rheumatoid Arthritis Patients. Cureus. 2022 Jan 15;14(1). Link
- Bavarian R, Khawaja SN, Ajisafe AH, Sultan AS. The efficacy of microcurrent electrical nerve stimulation in treating masticatory myofascial pain: A systematic review and meta-analysis. CRANIO®. 2021 Dec 24:1-7. Link
- Ferrillo M, Ammendolia A, Paduano S, Calafiore D, Marotta N, Migliario M, Fortunato L, Giudice A, Michelotti A, Sire AD. Efficacy of rehabilitation on reducing pain in muscle-related temporomandibular disorders: A systematic review and meta-analysis of randomized controlled trials. Journal of Back and Musculoskeletal Rehabilitation. 2022(Preprint):1-6. Link
- Khalighi HR, Mortazavi H, Mojahedi SM, Azari-Marhabi S, Parvaie P, Anbari F. The efficacy of low-level diode laser versus laser acupuncture for the treatment of myofascial pain dysfunction syndrome (MPDS). Journal of Dental Anesthesia and Pain Medicine. 2022 Feb 1;22(1):19-27. Link
- NAMVAR MA, AFKARI BF, MOSLEMKHANI C, MANSOORI K, DADASHI M. The Relationship between Depression and Anxiety with Temporomandibular Disorder Symptoms in Dental Students. Maedica A Journal of Clinical Medicine. 2021;16(4). Link
- Tuncer A, Atay F, Guzel HC, Tuncer AH. Comparison of factors affecting patients with a myofascial temporomandibular disorder with and without sleep bruxism. Nigerian Journal of Clinical Practice. 2022 Mar 1;25(3):273. Link
- Chew AQ, Saigo L, Yap AU. Is there a comorbid relationship between temporomandibular disorders and otologic signs/symptoms?: An umbrella review. CRANIO®. 2022 May 12:1-4. Link
- Silva TB, Ortiz FR, Maracci LM, Silva GB, Salbego RS, Liedke GS, Marquezan M. Association among headache, temporomandibular disorder, and awake bruxism: A cross?sectional study. Headache: The Journal of Head and Face Pain. Link
- da Silveira RB, Ferreira I, Botelho AL, Dos Reis AC. Effect of photobiomodulation treatment on pain control in patients with temporomandibular dysfunction disorder: systematic review. CRANIO®. 2022 Jun 17:1-1. Link
- Koparal M, Sirik M, Yavuz GY, Ege B. Evaluation of the Relationship between Temporomandibular Joint Disorders and Tinnitus with Computed Tomography. Journal of Stomatology, Oral and Maxillofacial Surgery. 2022 Jun 18. Link
- Maranini B, Ciancio G, Mandrioli S, Galiè M, Govoni M. The Role of Ultrasound in Temporomandibular Joint Disorders: An Update and Future Perspectives. Frontiers in Medicine. 2022;9. Link
- Koufos EB, Avila HC, Eckert G, Stewart KT, Kroenke K, Turkkahraman H. The TMD-7 as a Brief Measure for Assessing Temporomandibular Disorder. European Journal of Dentistry. 2022 Aug 9. Link
- Rezaie K, Amiri A, Ebrahimi Takamjani E, Shirani G, Salehi S, Alizadeh L. The Efficacy of Neck and Temporomandibular Joint (TMJ) Manual Therapy in Comparison With a Multimodal Approach in the Patients with TMJ Dysfunction: A Blinded Randomized Controlled Trial. Medical Journal of the Islamic Republic Of Iran. 1936 May;36(1):328-37. Link
- Ferrillo M, Nucci L, Giudice A, Calafiore D, Marotta N, Minervini G, d’Apuzzo F, Ammendolia A, Perillo L, de Sire A. Efficacy of conservative approaches on pain relief in patients with temporomandibular joint disorders: a systematic review with network meta-analysis. CRANIO®. 2022 Sep 24:1-7. Link
- Fredricson AS, Weiner CK, Adami J, Rosén A, Lund B, Hedenberg-Magnusson B, Fredriksson L, Naimi-Akbar A. The Role of Mental Health and Behavioral Disorders in the Development of Temporomandibular Disorder: A SWEREG-TMD Nationwide Case-Control Study. Journal of Pain Research. 2022 Sep 6;15:2641-55. Link
- Felin GC, da Cunha Tagliari CV, Agostini BA, Collares K. Prevalence of psychological disorders in patients with temporomandibular disorders: A systematic review and meta-analysis. The Journal of Prosthetic Dentistry. 2022 Sep 13. Link
- dos Santos Aguiar A, Moseley GL, Bataglion C, Azevedo B, Chaves TC. Education-enhanced Conventional care vs. Conventional care alone for Temporomandibular Disorders: a randomized controlled trial. The Journal of Pain. 2022 Oct 8. Link
112.Idáñez-Robles AM, Obrero-Gaitán E, Lomas-Vega R, Osuna-Pérez MC, Cortés-Pérez I, Zagalaz-Anula N. Exercise therapy improves pain and mouth opening in temporomandibular disorders: A systematic review with meta-analysis. Clinical Rehabilitation. 2022 Oct 20:02692155221133523. Link
- Uehara LM, Tardelli JD, Botelho AL, Valente ML, Dos Reis AC. Association between depression and temporomandibular dysfunction in adults-a systematic review. CRANIO®. 2023 Jan 8:1-7. Link
- Yamaguchi Y, Sakuma S, Ogi N, Taguchi N, Kimoto S. Short-term efficacy of exercise therapy for temporomandibular disorders: a case control study. Journal of Physical Therapy Science. 2023;35(2):139-45. Link
- Chew AQ, Saigo L, Yap AU. Is there a comorbid relationship between temporomandibular disorders and otologic signs/symptoms?: An umbrella review. CRANIO®. 2022 May 12:1-4. Link
- Serrano-Muñoz D, Beltran-Alacreu H, Álvarez DM, Fernández-Pérez JJ, Aceituno-Gómez J, Arroyo-Fernández R, Avendaño-Coy J. Effectiveness of Different Electrical Stimulation Modalities for Pain and Masticatory Function in Temporomandibular Disorders: A Systematic Review and Meta-Analysis. The Journal of Pain. 2023 Feb 18. Link
- Liu Y, Yin T, He M, Fang C, Peng S. Association of congenitally missing teeth with adult temporomandibular disorders in the urban health checkup population. BMC Oral Health. 2023 Mar 30;23(1):188. Link
- Shimada A, Ogawa T, Sammour SR, Narihara T, Kinomura S, Koide R, Noma N, Sasaki K. Effectiveness of exercise therapy on pain relief and jaw mobility in patients with pain-related temporomandibular disorders: a systematic review. Frontiers in Oral Health. 2023;4. Link
- Liberato FM, da Silva TV, Santuzzi CH, Nascimento LR. Manual Therapy Applied to the Cervial Joint Reduces Pain and Improves Jaw Function in Individuals with Temporomandibular Disorders: A Systematic Review on Manual Therapy for Orofacial Disorders. Journal of Oral & Facial Pain and Headache. 2023 Mar 1;37(2):101-11. Link
- de Melo Silva EM, Valdez RA, da Barbosa Silva IM, Chateaubriand MM, Duarte AL, Gueiros LA. Association between axial spondyloarthritis and temporomandibular disorders: A systematic review. Oral Diseases. 2023 Oct;29(7):2592-9. Link
- González-Sánchez B, García Monterey P, Ramírez-Durán MD, Garrido-Ardila EM, Rodríguez-Mansilla J, Jiménez-Palomares M. Temporomandibular Joint Dysfunctions: A Systematic Review of Treatment Approaches. Journal of Clinical Medicine. 2023 Jun 20;12(12):4156. Link
- González-Sánchez B, García Monterey P, Ramírez-Durán MD, Garrido-Ardila EM, Rodríguez-Mansilla J, Jiménez-Palomares M. Temporomandibular Joint Dysfunctions: A Systematic Review of Treatment Approaches. Journal of Clinical Medicine. 2023 Jun 20;12(12):4156.
- Gobska M, Dalewski B, Paka, Kiczmer P, Koodziej. Effect of physiotherapeutic procedures on the bioelectric activity of the masseter muscle and the range of motion of the temporomandibular joints in the female population with chronic pain: a randomized controlled trial. BMC Oral Health. 2023 Nov 25;23(1):927. Link
- Bednarczyk V, Proulx F, Paez A. The effectiveness of cervical rehabilitation interventions for pain in adults with myogenic temporomandibular disorders: A systematic review and meta analysis. Journal of Oral Rehabilitation. 2024 Mar 7. Link