As one who treats the movement systems (neuromusculoskeletal), I have several tools at my disposal: joint mobilization, spine and joint manipulation, soft tissue manual therapy, stretching, stabilization exercises, instrument assisted soft tissue manipulation, kinesiotaping, athletic taping, dry needle therapy, ice massage, traction, corrective exercise, education, listening, and encouraging (to name a few). The problem is that some people assume that the treatment tool is actually a treatment system. If home construction were the same way, that would be like looking for a builder that specializes in the “hammer system”, because you’ve heard that nails are the best for building a strong house. When in fact, you want a well-equipped professional to explain what it’s going to take to help you reach your goals.
In order to help someone towards their health goals, we need to apply the right combination of tools, in the right way, at the right time, for the right diagnosis.

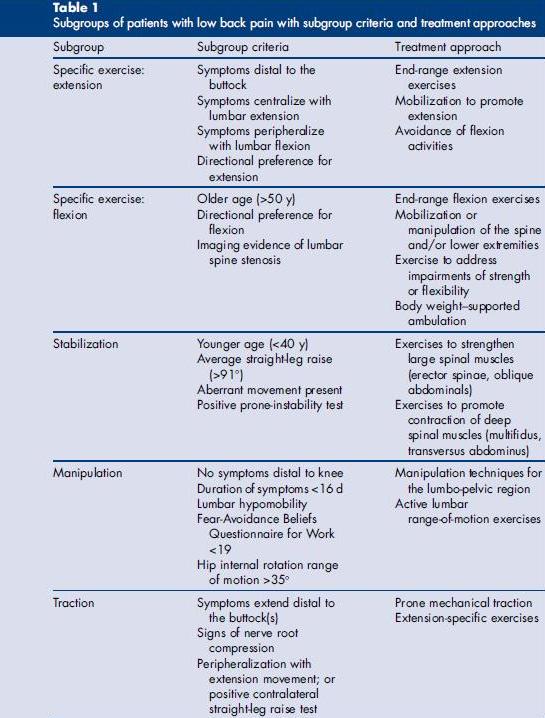
More recently, research into the rehabilitation of neuromusculoskeletal pain syndromes has investigated which patient characteristics predict success with a certain treatment. An article entitled Clinical Prediction for Success of Interventions for Managing Low Back Pain (Clin Sports Med) summarizes some important findings.
This paper summarizes the aggregate result of other high quality studies, reporting the most significant factors determining success. It is not intended to be a paint-by-number algorithm, but does give some interesting data. If a patient fulfills the criteria for one subgroup, it does not mean that treatments best for other subgroups should be avoided. For example, if someone with back pain meets 3 of the top 4 criteria in the “manipulation” subgroup, there is a 95% probability of a successful outcome (Fritz J, Whitman. Arch Phys Med Rehabil, 2005). Yet if the patient doesn’t meet any of the “manipulation” group criteria, there is still a 45% probability for success! ( Flynn T, Fritz J et al. Spine, 2002). Clearly the best outcomes come from the evidence-based application of a variety of treatments.

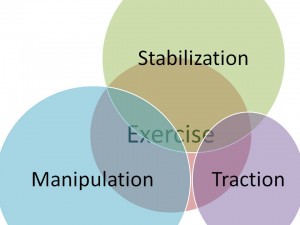
And what about treatment timing? It’s my opinion the diagram to the left represents a logical progression of treatments that would get the most sustainable improvements in both pain and function over the shortest amount of time. Let’s look at a specific example to see how this progression would work.
Jane (not a real name) came to Cole Pain Therapy Group with 3 weeks of low back pain that occasionally radiated to the right lower leg. She explained that the pain was worse while stooping over to care for her infant son. She had been stretching her hamstrings, which felt tight, to no lasting benefit. Her goal was to get out of pain and be able to function through the busy day. Eventually she hoped to get back to boot camp style training for weight loss, but feared her back would never be strong enough.
After our discussion, the examination revealed several pertinent features for this example:
- Pain radiated from the back to the leg with repeated forward bending
- Pain improved with low back extension
- She was 28 years old (an easy one to figure out)
- She had an altered movement pattern
- The straight leg raise was >91 degrees
So from consulting the table above, she fulfilled criteria to fit into the “specific exercise- extension” and “stabilization” subgroups. Treatment isn’t limited to these groups, but the best rehabilitation science available strongly suggest including extension exercise and stabilization into her treatment plan. The pictures below illustrate the progression of treatment.
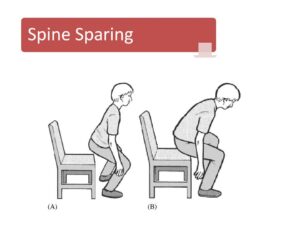
1st session. Instruction about how to move in a way that doesn’t hurt. Jane was squatting/stooping better within 5 minutes, feeling more confident since it didn’t make her back hurt like before.
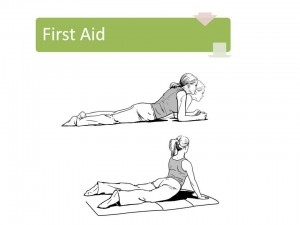
More at 1st session. She was instructed on McKenzie extension exercises to be performed 10x/ day for the next 2 weeks (McKenzie Self Treatment Handout). She also received spinal manipulation to improve spine function and ultrasound with e-stim for pain control.
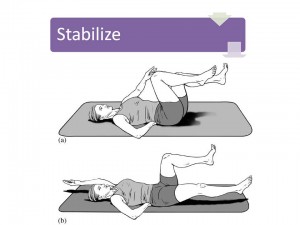
Start and finish positions for a customized exercise that develops spine stability in the context of hip and shoulder mobility. Sessions 7- 10. She was instructed and performed a variety of stabilization exercises. The focus of these customized movements was to train stability at the core (her God-given back brace) in the context of motion at the hips and shoulders. It is not a matter of strength, but of control. I also applied spine manipulation to improve mid-back mobility and applied kinesiotape to support a related shoulder blade tracking problem.
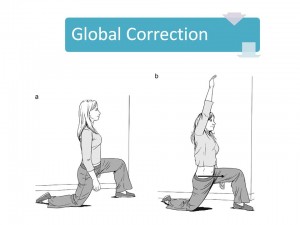
More at sessions 7-10. When normal movement was no longer painful, she went through a series of functional movement screens to uncover dysfunctional movements that were not necessarily painful. The above corrective exercise was prescribed in order to correct a predisposing factor to the original low back pain episode. So the purpose of global correction is to address movement problems remote from the site of pain. It’s these silent dysfunctions that derail fitness goals.
After the last session, she returned to the office every 4-6 weeks per her goals to address minor pains or movement issues and to discuss the application of her customized stability principles in the context of her boot camp training. Since she knew how to check her own movement performance via self-audit, she was able to train more confidently. Building durability involves the above five steps proposed by author and researcher, Dr. Stewart McGill.
This post is based on a presentation that I was pleased to deliver at the 2013 ChiroAdvance symposium. Thanks to Dr. Kevin Foley, Dr. Autry Parker, Dr. Ron Fudala, Dr. Bruce Fox, Dr. Jeff Luebbe, and Dr. David Schimp for graciously sharing the lectern.