The majority of neck pain cases are due to a failure of the movement system. To effectively treat the pain, one must look outside of the neck to assess the function of the entire movement system.
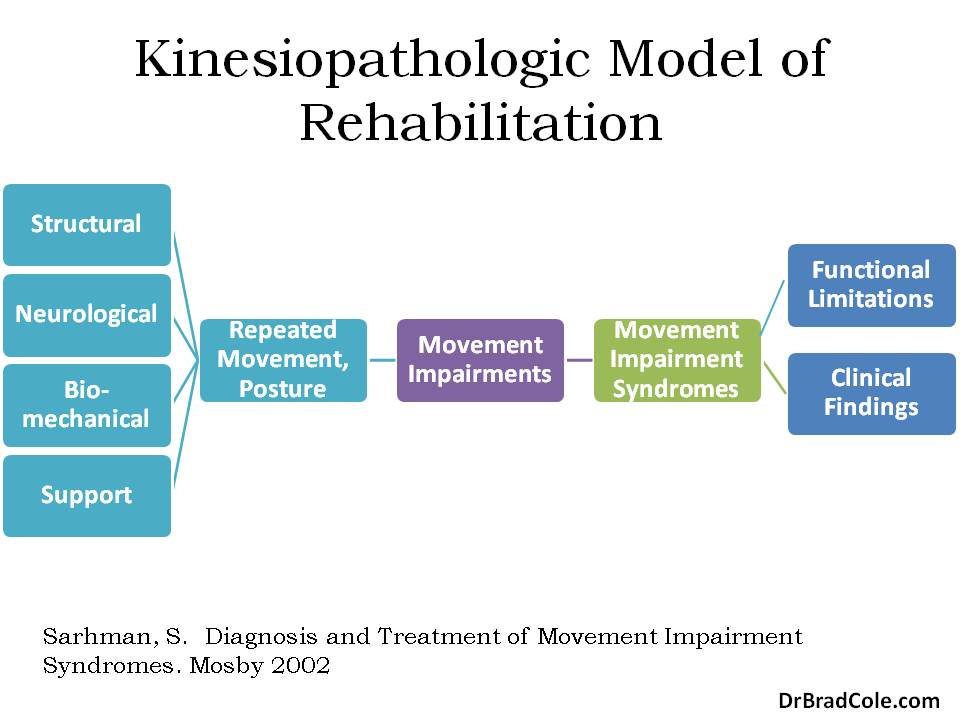
Professor Sahrmann’s first textbook regarding functional impairments explains the kinesiopathologic model rehabilitation. This model attributes degeneration, pain, and limited function to stereotypical patterns of movement dysfunction. Given the fact that we as humans develop our movement system from a genetically predetermined neurodevelopmental process, dysfunctions in the motor system occur in predictable patterns.
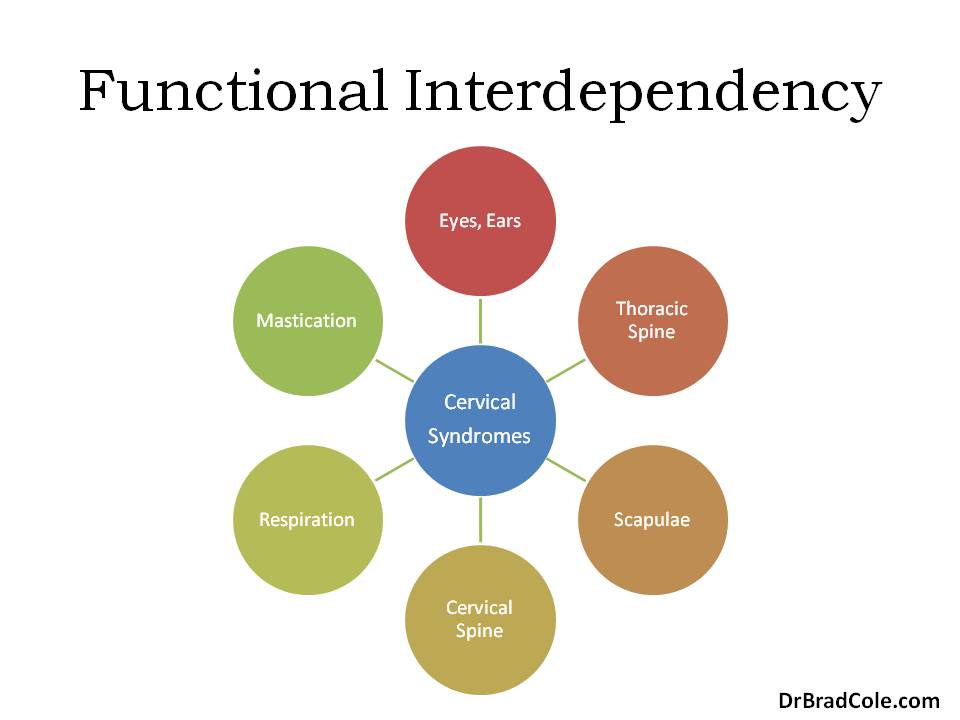 Functional movement impairments that result in neck pain are affected by the sensory system, mastication, respiration, cervical spine, upper extremities, and trunk. Any functional evaluation should be performed in deference to this principle of functional interdependency.
Functional movement impairments that result in neck pain are affected by the sensory system, mastication, respiration, cervical spine, upper extremities, and trunk. Any functional evaluation should be performed in deference to this principle of functional interdependency.
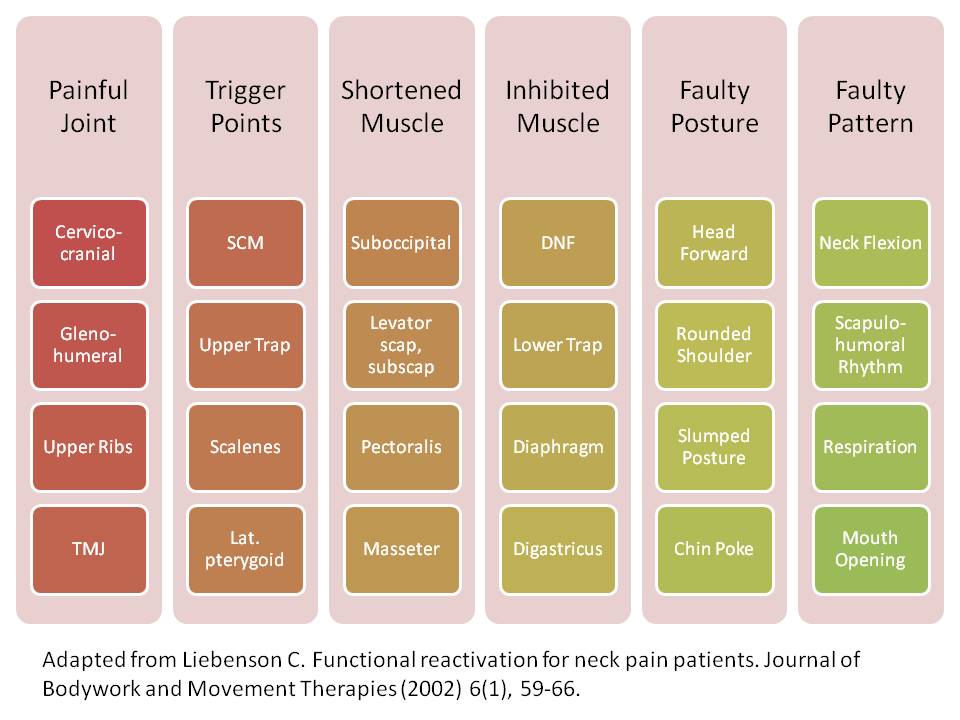
Dr. Craig Liebenson’s paper entitled Functional Reactivation for Neck Pain Patients (message me and I’ll send it to you) outlines stereotypical patterns of movement system dysfunction which may be affecting the cervical spine. Without acknowledging these patterns of dysfunction, there is no clinical roadmap for rehabilitation. One ends up treating a patient’s symptoms with a “whack-a-mole” philosophy – simply addressing whichever may be painful from episode to episode. One should ultimately address the faulty pattern.
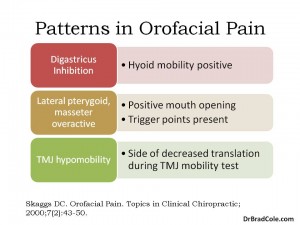 Similarly, cervical and craniofacial pain syndromes often involves the masticatory system. Assessing this system does not take very long and can be easily included in the standard examination of any new case of neck, face, or head pain. Since the majority of craniofacial and cervical spine pain is functional, we should all be vigilant in having a rehabilitation roadmap in order to provide what research has shown to be the best care. Manual medicine and rehabilitation is clinically effective, cost effective, and encouraging to those in pain.
Similarly, cervical and craniofacial pain syndromes often involves the masticatory system. Assessing this system does not take very long and can be easily included in the standard examination of any new case of neck, face, or head pain. Since the majority of craniofacial and cervical spine pain is functional, we should all be vigilant in having a rehabilitation roadmap in order to provide what research has shown to be the best care. Manual medicine and rehabilitation is clinically effective, cost effective, and encouraging to those in pain.
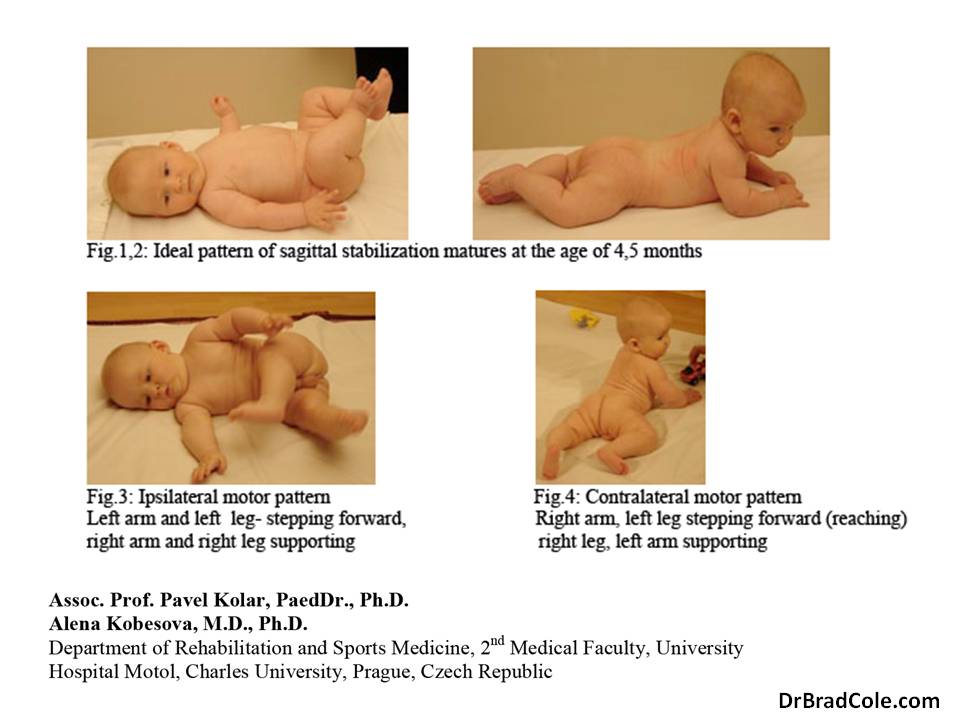
Pavel Kolar, PaedDr, PhD and Alena Kobesova, MD, PhD eloquently describe the need for functional norms in the evaluation of musculoskeletal pain. Clinicians are familiar with norms when it comes to laboratory testing, physical evaluation, etc. Unfortunately, researchers have had a difficult time isolating functional norms or musculoskeletal pain. Pain fails to correlate with deficits in strength or range of motion.
The concept of dynamic neuromuscular stabilization (DNS) is that normative neurodevelopment reveals functional norms for all individuals. The figures below illustrate ideal patterns of sagittal stabilization in the supine and prone positions. Additionally, all human locomotion follows a contralateral or ipsilateral pattern. Understanding these appropriate patterns allows the clinician to then compare at patient’s movement quality to that which is dictated by ideal physiology.
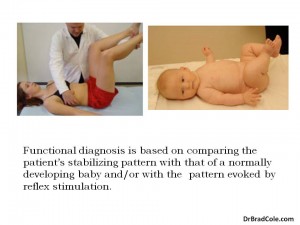
In the developing infant, sagittal stabilization occurs prior to intentional movement of the arms, legs and head. By studying pediatric neurodevelopment, we can then have functional norms of stabilization to guide treatment of both infants and adults. (Read Postural Locomotion Function in the Diagnosis and Treatment of Movement Disorders)
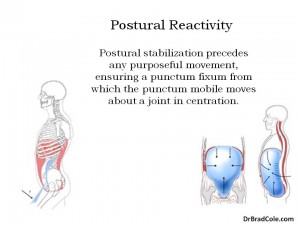
By our bodies position and interaction with our environment, we have reflex activation of postural muscles so that movements occur in a stable, centrated position. Joint concentration allows for optimal distribution of forces across the joint. When an individual is growing, this creates the joint’s morphology. This is why altered neurological development also results in altered musculoskeletal development.
To maintain joint centration, prior to any movement, there is an automatic postural stabilization occurring via low-grade activity of the intra-abdominal pressure system and deep spinal stabilizers.
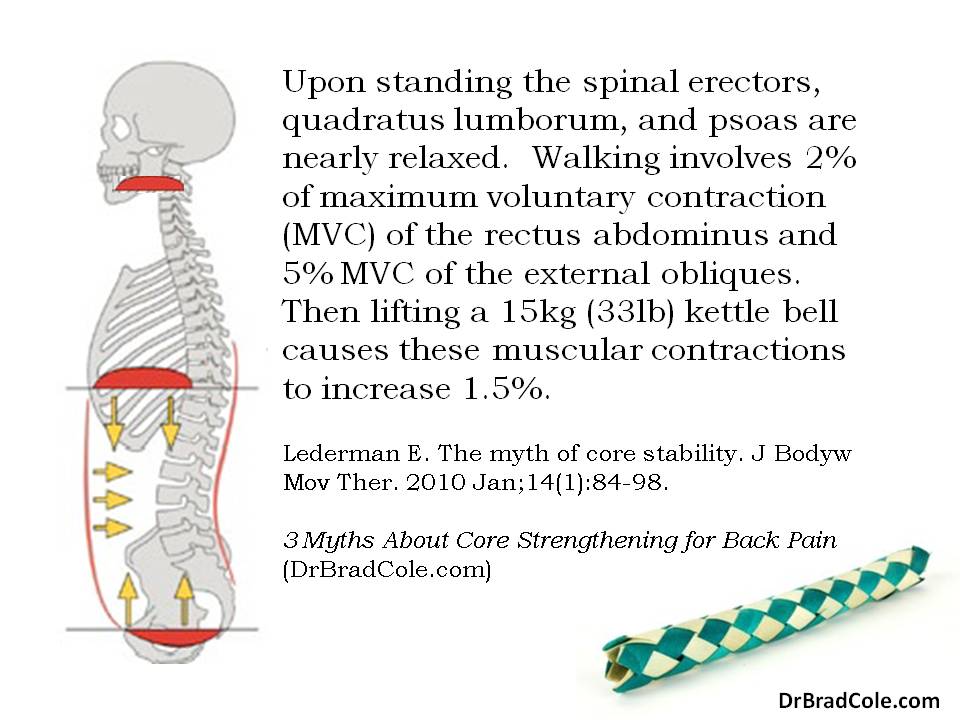
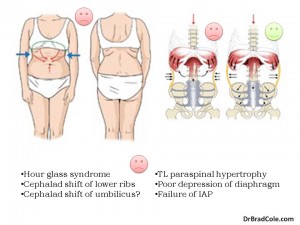 When there is poor synergy between the abdominal muscles, postural and movement dysfunction results in a predictable pattern. In the case of an “hourglass” postural dysfunction, the rib cage fails to expand laterally and shifts up and down during respiration. This results in failure of the intra-abdominal pressure system and over activity of the upper respiratory muscles. One of the many symptoms that results from this cascade of dysfunction is pain and degeneration of the cervical spine.
When there is poor synergy between the abdominal muscles, postural and movement dysfunction results in a predictable pattern. In the case of an “hourglass” postural dysfunction, the rib cage fails to expand laterally and shifts up and down during respiration. This results in failure of the intra-abdominal pressure system and over activity of the upper respiratory muscles. One of the many symptoms that results from this cascade of dysfunction is pain and degeneration of the cervical spine.
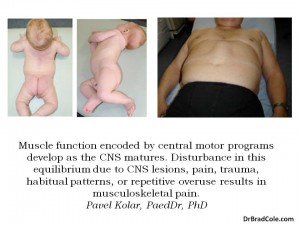
Muscular morphology and function encoded by central motor programs develop with the maturing central nervous system. Therefore, altered function of the movement system may result from CNS lesion, pain, trauma, habitual pattern, and repetitive movement. Because central motor programs are stereotypical, disturbance of the program results in stereotypical patterns of dysfunction.
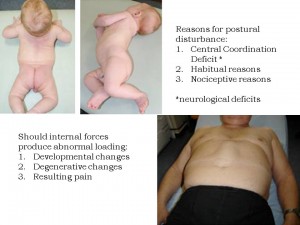
We can see with the figures to the left that impaired sagittal stabilization in the prone and turning infant may result in altered morphology of chest wall, function of abdominal muscles, and quality of movement in the supine adult lifting his head.
Since ideal, automatic postural stabilization must precede quality movement, any rehabilitative treatment for abnormal development, physical degeneration, and musculoskeletal pain must be performed in deference to the deep stabilization system.

Quality movement is efficient. Ultimately, this results in proper development, less degeneration, and greater durability of the human frame. The athlete in blue is demonstrating optimal joint centration, similar to that of a normal developing baby. On the other hand, the athlete in purple is demonstrating failure of the sagittal stability system. She may do well with activation of the intra-abdominal pressure system in the supine position to practice the automatic pattern of ideal stabilization with which she was born.
This article is an excerpt of a presentation Functional Assessment and Rehabilitation of the Cervical Spine (Midsouth Cervical Spine Symposium; January 18-19, 2014)